COVID-19 Natural Immunity: a deep dive
How does natural immunity compare to vaccine-induced immunity?
Dr. Ezekiel Emmanuel: “Is a person likely to be immune once they caught the coronavirus once? Do we know anything about likely drift?”
Dr. Anthony Fauci: “You would assume that their [sic] would be substantial immunity post infection.”
- Email exchange March 4th, 2020, via FOIA
Nearly two years into this pandemic, we still don’t have a clear answer to this basic question:
Is a previously infected person less, equally, or more protected than a vaccinated one?
With all the advocacy and campaigning to encourage widespread vaccination, it has been difficult to tease out exactly how strong natural immunity really is. The dean of Brown University School of Public Health Dr. Ashish Jha argued that natural immunity “likely wanes” after 3 months, and wanes “certainly after six months” in a Twitter thread attempting to explain why vaccinated individuals continue to be far better protected. While the vaccines remain highly effective at reducing severe illness, he compares their effectiveness to population data of unvaccinated people that does not specify who has natural immunity and who does not.

Experience with prior viruses suggests we do in fact have lasting immunity to many of them. People born prior to 1918 that are still alive, for example, amazingly still have neutralizing antibodies to the 1918 flu pandemic strain.
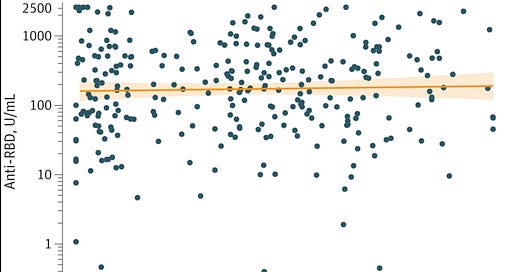
While we don’t have 105-year data for SARS-CoV-2, we do now have many studies looking at natural immunity up to two years. Most recently was a Johns Hopkins study that checked antibody levels in people previously infected but not vaccinated. Antibody levels alone do not prove protection from severe disease, but they are highly suggestive of it.
They found that 99% of people who were previously infected had antibodies up to 20 months out (median of 8.7 months). 44% had levels ≥250, 27% had levels ≥500, and 15% had ≥1000, which, based on Moderna vaccine antibody targets, corresponds to vaccine efficacy of 91% or greater.

Very similar results were seen in a study published in Nature that touts a 16-month follow-up in 214 infected people who had not been vaccinated. Neutralizing antibodies reached their peak around 120 days, decreased slowly, and remained stable after 400 days at levels that would protect against severe disease and reinfection for most people in the study.

They also found that the magnitude of the antibody response was dependent on the severity of infection, with the highest titers seen in people who had severe disease, and the lowest in those who were largely asymptomatic. In fact, 14% of mild and 50% of asymptomatic infections had no detectable antibodies after 330 days, and would presumably no longer be protected.
These studies are incredibly important for elucidating how we can more objectively determine if someone is immune, and offer individually tailored recommendations rather than blanket statements for all (i.e. “Everyone should get a booster”). These studies did not look at outcomes like reinfection or death, but many other studies have, and they all seem to find the same conclusion: natural immunity is as good (or maybe even better) than vaccine-induced immunity. For example:
A Cleveland Clinic study of 52,238 healthcare workers between Dec 2020 to Dec 2021 found that both vaccinated and those previously infected had similar protection, with 99% of re-infections occurring in those who were not immune.
A year-long study looked at re-infection rates at Curative, a SARS-CoV-2 testing company, and found that the natural immunity group had an infection rate of 0 per 100 person-years, compared to 1.6 per 100 person-years in the vaccinated group, and 25.9 per 100 person-years in the unvaccinated, non-immune group. They concluded that “either prior infection or vaccination was associated with a dramatic decreased risk for infection or re-infection with SARS-CoV-2. There was no difference in the incidence of SARS-CoV-2 infection or re-infection between individuals who were vaccinated and individuals with prior SARS-CoV-2 infection, respectively.”
A retrospective study of 150,325 patients similarly found an 83% risk reduction against symptomatic disease and 78% against all infections in those previously infected. Few patients were hospitalized following reinfection, and none with COVID-related symptoms required intensive care. Six months after infection, protection against symptomatic disease exceeded 90%.
A New England Journal of Medicine study from February 2021 looking at reinfection rate in over 12,000 healthcare workers with 6 month follow up found that natural immunity reduced risk of reinfection by 89% (graph below)
A large 2020 Danish study found an 80% risk reduction in the natural immunity group, with a rate of 5.35 per 100,000 compared to 27.06 per 100, 000 in those who were not immune.
Previous infection also reduced the risk of reinfection by 93% in a large study in the New England Journal of Medicine, and those that were re-infected had 90% lower risk of being hospitalized.
A large Israeli study with from June to Aug 2021 found that the vaccinated (or not previously infected) group had a 13x higher risk of reinfection and 27x higher risk of symptomatic infection when compared to the previously infected group.
Waning immunity
With vaccine-induced or infection-induced immunity, we should expect the antibody levels to reduce to some degree, but by how much and compared to what? From August to September 2021, Israeli researchers performed another study during the Delta wave, comparing the re-infection rates in those who either recovered from COVID-19 and did not get vaccinated, recovered from COVID-19 and then got vaccinated, or in those who were never infected and got vaccinated and boosted. Surprisingly they found that while all groups had waning immunity, those who were vaccinated and boosted had the worst protection from reinfection at 6 months:
Natural immunity group: The rate of infection increased from 10.5 per 100,000 to 20 per 100,000 at 6 months, to 30 per 100,000 risk-days after 12 months.
Prior infection + Single dose: Increased from 3.7 per 100,000 person-days to 11.6 for those vaccinated over 6 months ago.
Vaccinated previously uninfected: the rate per 100,000 person-days increased from 21.1 for persons vaccinated within the first two months to 88.9 for those vaccinated more than 6 months prior

So at 6-8 months post-infection the natural immunity group had a re-infection rate of 20 per 100,000 while the vaccinated and boosted were at 90 per 100,000. So - at least according to these studies - while Dr. Jha was correct that natural immunity wanes at 6 months, it seems to reduce less than the vaccination with booster, something the CDC finally accepts as well.
Finally, a systematic review on the topic concluded that while “vaccinations are highly effective at protecting against infection and severe COVID-19 disease … natural immunity in COVID-recovered individuals is, at least, equivalent to the protection afforded by full vaccination of COVID-naïve populations. There is a modest and incremental relative benefit to vaccination in COVID-recovered individuals; however, the net benefit is marginal on an absolute basis.”
Therefore, it seems clear that, at least in the first few months (and likely up to 2 years or more), natural immunity is similar - and likely better - than vaccine-induced immunity.
Does this hold up in the Omicron Era?
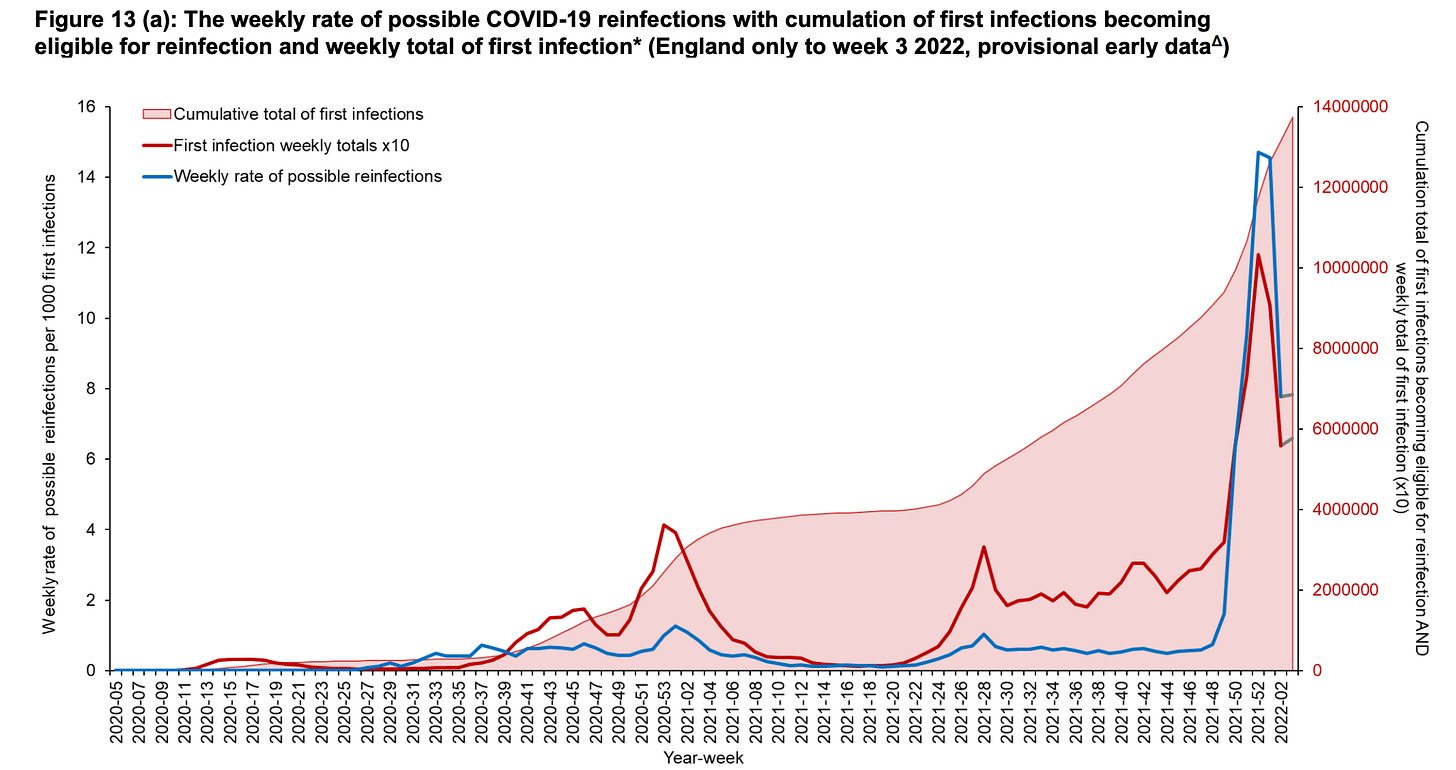
Yes and no. Vaccines and previous infections do not seem to reduce your risk of getting infected with Omicron, as was abundantly clear by cities, states, and countries with record case counts despite 90%+ vaccination rates. This figure on re-infection from the U.K.’s weekly influenza and COVID-19 report says it all. (Blue spike is Omicron):
While they clearly don’t prevent Omicron infections, the vaccine-induced immunity continues to be incredibly effective for preventing severe illness. This roughly 90% reduced risk has been corroborated by different hospitals, in different countries with many different patient populations.
Vaccines after infection
So if natural immunity is so strong, how does vaccination affect the level of immunity if you’ve already been infected? Antibody titers after the first dose of mRNA in people with previous infection were 10 to 45 times higher in one study, compared to those who were not previously infected, and were 6x higher than the antibody levels after the second vaccine dose in people without previous infection. This may explain why people with a history of COVID-19 reported greater rates of side effects after vaccination.
The CDC’s own data suggests that vaccination after natural infection does not provide additional reduction in hospitalizations, so maybe it is time to take a more personalized approach, as has been proposed by transplant surgeon Dr. Dorry Segev:
“Instead of just guessing, or assuming “one size fits all” (we saw what a disaster it caused when we assumed immunocompromised patients had the same response as everyone else), we can now test antibody levels and recommend boosters when levels fall below some threshold. We can even choose different thresholds for people of different risk profiles: If you have a higher risk of exposure to SARS-CoV-2 (or exposing others) because of your job, or if you have a higher risk of getting very sick with COVID-19 because of your comorbidity profile, you should get boosted at a higher antibody level. B if you have minimal exposure and are otherwise quite healthy, you could wait to reach a lower antibody level before boosting. This individualized approach would optimize protection while making the best use of available vaccine doses.”
Does someone who had mild or asymptomatic infection have protection at 6 months? What about someone over 70? What about someone who had two vaccines and then got omicron asking about the need for a booster? Should those previously infected get one mRNA dose or two? All these questions could be answered with a reliable quantitative antibody test, which LabCorp now offers.
—
Dr. Istrail is the author of The POCUS Manifesto: Expanding the limits of our physical exam with point-of-care ultrasound. You can get a copy here.




"While the vaccines remain highly effective at reducing severe illness," are they really?!
This type of statement seems just as absurd as saying "While face masks remain highly effective at reducing the rate of transmission"!
The cattle farm where I exist is one of the "countries" you refer in the article.
Today, Feb 10th, we have 91,22% of the cattle inoculated with 2 doses, and 55,09% with 3 doses.
Now to the FUN part...
If we consider in this scenario that death occurs on the severely ill (no reason to consider that death occurs on a mild case or even on the asymptomatic) the real life evidence (this naturally excludes the pharma studies made in-house) shows that these inoculations aren't "highly effective at reducing severe illness"
Official data for the cattle farm Portugal:
From 17Mar2020 to 26Dec2020 (285 days) WITHOUT "vaccine": average daily deaths with PCR tag "COVID-19" - 23
From 27Dec2020 to 07Oct2021 (also 285 days) WITH "vaccine": average daily deaths with PCR tag "COVID-19" - 40
So for the same period of time we can see that the introduction of the "vaccine" caused more deaths, which means caused more severe illness.
And if we continue to follow the count not even more days can do the trick!
From 27Dec2020 to 04Feb2022 (405 days!) WITH "vaccine": average daily deaths with PCR tag "COVID-19" - 34
So unless the "vaccine success" is being viewed from the "culling the cattle" perspective, it clearly does't look that the above statement is adequate.